Conditions
Carotid Endarterectomy
A carotid endarterectomy may be performed if you have had a TIA (mini-stroke), a sudden loss of vision in one eye (Amaurosis Fugax), or a major stroke. These conditions are due to carotid artery disease, the narrowing of one (or both) of the main arteries, located in your neck, supplying blood to your brain. Alternatively, you may be offered this type of surgery if a significant narrowing or ulcer is detected in the carotid artery before it had a chance to cause any symptoms. This is often discovered in some people during the conduct of investigations for another problem. If that is the case for you, you will still undergo the same preoperative tests, but you will be admitted to hospital for surgery in a less pressing or urgent manner.
The whole objective of carotid endarterectomy is to prevent you having a major debilitating / lethal stroke.
Before you have carotid surgery, there are a number of tests which need to be done to assess whether you are able to have the operation, such as:
- Ultrasound (Triplex) scan
- MRA or a CT-Angiogram with injection of dye in the blood to look at the anatomy in detail
- Blood tests
- ECG (a heart tracing)
- Echocardiogram (an ultrasound test of the heart) and you will have a cardiology review Imaging (MRI) of your brain.
If you are fit enough, you will then be offered an operation. Your surgeon will very likely ask you to take both Aspirin and Clopidogrel, among other medication, even the day before the operation. Discuss your medication with your surgeon.
Carotid endarterectomy can be performed under either “local” or general anaesthetic. Not all cases are suitable for avoiding the general anaesthetic. In particular patients who are very anxious should prefer a general anaesthetic. Your surgeon will advise you as to which method of anaesthetic you will be offered.
For a general anaesthetic, a tiny needle is placed in the back of your hand. The anaesthetic is injected through the needle and you will be asleep within a few seconds.
For local anaesthetic, the Anaesthetist will make an injection into the skin of your neck to numb it and also slightly deeper to numb the deeper tissues. During the operation, if you become uncomfortable, the surgeon will inject more local anaesthetic. You will also be given some sedation, and as a result, you may not be very aware of the operation at all. Occasionally it may be necessary to convert to a short general anaesthetic during the operation.
A tube (catheter) may be inserted into your bladder to drain your urine.
A drip is placed into a vein in your arm (wrist usually) to give you some fluids during and following surgery. Frequently, a second drip will be placed into an artery at wrist level to permit careful blood pressure monitoring during and just after the operation.

You will have a cut running obliquely down from near the angle of your jaw / ear lobe towards your breastbone. The inci- sion is usually 7-10cm in length.
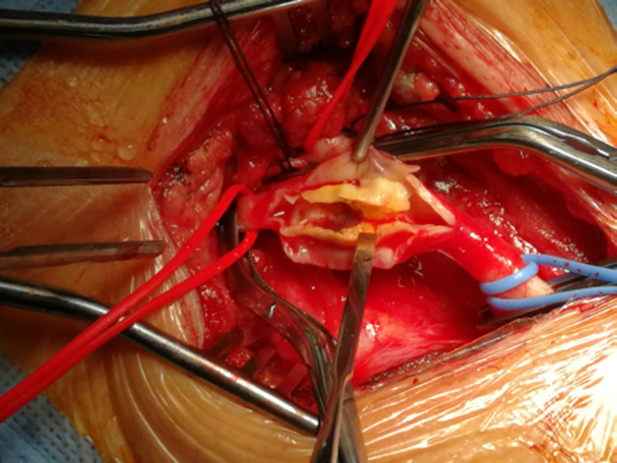
Once the carotid artery is displayed, the branches of the artery are clamped to limit blood loss during the operation. A small incision is made along the artery and the plaque (the “narrowing”) is carefully removed.
To protect the brain from interruption to its blood supply while the artery is clamped, a shunt (narrow plastic tube) is sometimes used to maintain blood flow. The shunt lies in a loop outside the artery, passing into the artery above and below at each end of the incision in the artery.
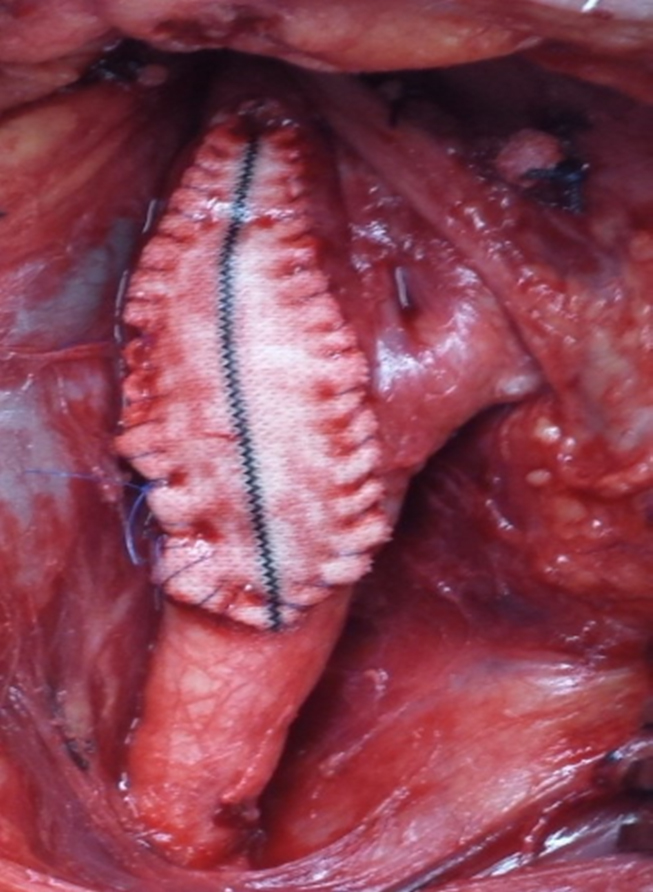
When the inside of the artery has been cleared, it is closed with very fine stitches. A small patch will usually be stitched to the artery to prevent further narrowing. This patch is normally made of a material called Dacron as shown in the picture.
The wound is usually closed with a stitch under the skin that dissolves. Your surgeon will place a small plastic drain in your neck for a short period to get rid of minor bleeding that collects after the operation, to reduce neck swelling and inev- itable bruising after the operation.
You will be taken to the High Dependency Unit for up to 24 hours after your operation so that your progress can be closely monitored.
You will wake up immediately at the end of the operation (if it has been under general anaesthetic). Local anaesthetics are used to numb the skin in all cases so there should be little discomfort.
Following this sort of surgery you are unlikely to feel sick, and you should be able to eat and drink again within a few hours. Your mobility will return to normal more or less immediately.
There is often some swelling and bruising in the neck, but this settles within 10 - 14 days.
The incision on your neck will initially be very visible; however this will subside to become virtually invisible within 3-6 months.
Most people stay in hospital between 2 and 4 days after carotid endarterectomy. The commonest issue for delays is having a very low blood pressure after the operation. This is because the brain is getting much more blood after the narrowing has been cleared, and it takes a little while for the brain to get used to it. You will be discharged from hospital when your blood pressure is adequate and you do not feel dizzy when standing.
If your stitches or clips are the type that need removing you will be advised how to have them removed later in clinic. Absorbable sutures will not need to be removed – ask your doctor which type you have. Regular exercise such as a short walks combined with rest is recommended to provide a gradual return to normal activity. Drink plenty of water, as advised by your doctor, to keep your blood pressure high enough, but not too high! (lowest acceptable is 110 mmHg and highest acceptable is 155 mmHg).
Driving: You will be able to drive when you can perform an emergency stop safely and look over your shoulder easily. This will normally be 2-3 weeks after surgery, but if in doubt check with your doctor. You should inform your insurers that you have had this operation.
Bathing: Once your wound is dry after 4-5 days you may bathe or shower as normal.
Work: If this applies to you, you should be able to return to work within 3-4 weeks of surgery. Your doctor will advise you of this when you see him/her for your sick-note.
Lifting: There are no limitations in this area.
Medicines: You will usually be sent home on a small dose of aspirin and clopidogrel, both of which very likely you had already been taking. This makes the blood less sticky. If you are allergic to aspirin, or if it upsets your tummy, an alternative drug may be prescribed. No other changes to your medication are required, except perhaps regarding the blood pressure, which will be discussed with your surgeon.
Worldwide, current guidelines recommend Carotid endarterectomy as the main
treatment for narrowing of the carotid arteries. An alternative procedure,
which does NOT in- volve open surgery (a cut in the neck) is called carotid
artery stenting. This is offered as part of randomised trials that are still
ongoing or when the patient is too high a risk for open surgery due to other
medical issues (e.g. previous radiotherapy or surgery to the neck, very high
carotid lesion going to the base of the skull and thereby being surgically
dif- ficult to get to).
Although the procedure of carotid stenting may appear less invasive because
it does not involve a surgical cut, in fact it has been shown to be
associated with a higher risk of stroke during the procedure, compared to
Carotid Endarterectomy, particularly if the stenting is done in the first
few days after symptoms appear and in patients over the age of 70.
Carotid stenting involves passing a wire through a small cut in the groin,
up through the carotid narrowing and then placing a wire-mesh, hollow
cylinder-shaped structure (stent) in the narrowed section, stretching it so
that the mesh pushes the plaque into the arterial wall to make the passage
wider. The stent gets slowly incorporated inside the wall of the artery.
Stroke: A small number of people, between 1 and 3 in 100,
having carotid endarterectomy will have a stroke during the operation. This
severity of stroke can be very mild, causing little or no disability,
through to severe causing major disability and death. All possible
precautions will be taken to prevent this eventuality.
Other Major Complications: As with any major operation
there is a small risk of you having a medical complication such as a heart
attack, kidney failure, chest problems, or infection in the wound. Each of
these is rare, but overall it does mean that some patients may have a fatal
complication from their operation. For most patients this risk is about 2% -
in other words 98 in every 100 patients will make a full recovery from the
operation. If your risk of a major complication is higher than this, usually
because you already have a serious medical problem, then your surgeon will
discuss this with you. It is important to remember that your surgeon will
only recommend treatment if he believes that the threat of stroke without
operation is much higher than the threat posed by the operation itself.
Chest infections:
These can occur following this type of surgery, particularly in smokers and
may
require treatment with antibiotics and physiotherapy.
Wound infection:
Wounds sometimes become infected and this may need treatment with
antibiotics.
Wound infections for this type of procedure are rare. Infection of the patch
inserted is a very rare, but serious complication, which necessitates repeat
surgery and is a threat to life.
Fluid leak from wound:
Occasionally the wound can bleed or bleeding beneath the wound will cause
swelling. Usually the swelling will settle on its own, but occasionally the
wound may need further surgical attention. Being on 2 blood-thinners
(aspirin
and clopidogrel) protects you from having a stroke but you may be at an
increased risk of bleeding that may require a return to theatre.
Nerve injuries:
These are uncommon. Skin nerves are interrupted by the incision leading to
some
loss of skin sensation, which by and large recover over time. Nerves nearer
the
carotid artery often have to be moved out of the way to complete the
operation
and that can lead to temporary, and rarely permanent loss of function. The
vagus
nerve provides a branch to the voice box (larynx) leading to a hoarse
sounding
voice. The hypoglossal nerve supplies the muscles of the tongue affecting
speech
slightly by reducing the tongue’s mobility. The facial nerve sup- plies the
muscles of the face. Damage to its lowest branch may lead to impaired
movement
of muscles around the lower jaw and neck.
If you are a smoker you MUST make a determined effort to stop completely.
Continued smoking will cause further damage to your arteries and increase
the risks of heart attacks, strokes, and problems with the circulation in
your legs. You should eat a low fat diet, avoiding food with high saturated
fat content and take regular exercise.
Talk to your doctor about controlling your cholesterol. All patients who
have a Carotid Endarterectomy MUST be on a statin, if they are not allergic
to it.